Traditional (relaxation) massage and medical (clinical) massage serve distinct goals. Traditional massage focuses on stress relief and comfort, while medical massage targets diagnosed musculoskeletal problems to reduce pain and restore function. This guide explains each approach, who benefits, and how to choose the right therapy. Many confuse spa treatments with clinical care, which can delay recovery. This guide offers clear definitions, examples, and decision tools to match symptoms with the most appropriate option. We compare techniques, settings, and insurance, showing how integrated clinics improve results. Read on for practical next steps and quick decision aids for focused treatment.
What Is Traditional Massage and What Does It Do Best?
Traditional massage, often called relaxation or spa massage, uses rhythmic strokes and light-to-moderate pressure to ease muscle tension and activate the body’s rest-and-digest response. It improves circulation, lowers arousal, and promotes calm. Benefits include reduced stress, temporary muscle loosening, mood improvement, and fewer tension headaches. People commonly book traditional massage to unwind, relieve tightness, or support general wellness.
How Does Traditional Massage Produce Relaxation?
Traditional massage calms the nervous system with slow, rhythmic touch, promoting parasympathetic activity like slower heart rate and lower blood pressure. This sensory input reduces cortisol and raises relaxation markers. Better local circulation also reduces tissue stress, experienced as less tightness. A typical visit combines comfort checks, flowing strokes, and therapist adjustments based on feedback to produce immediate relief, often improving sleep and daily recovery.
For ongoing stress management, clients pair routine traditional massage with home habits. This contrasts with medical massage, where the aim shifts to measurable, lasting improvement.
Common Techniques in Traditional Massage
Traditional massage uses modalities chosen for comfort and relaxation, not structural correction. Swedish massage uses effleurage and petrissage for circulation; hot stone therapy applies heat to relax tissue; aromatherapy-enhanced sessions combine hands-on work with essential oils for emotional calm. Technique selection is guided by client preference and desired relaxing effect, not by diagnostic examination.
Sessions generally run 30–90 minutes, prioritizing atmosphere and comfort. Therapists adjust pressure to keep the experience relaxing. Knowing which techniques emphasize relaxation helps you decide when a spa-style session is appropriate.
What Is Medical Massage and What Are Its Therapeutic Benefits?
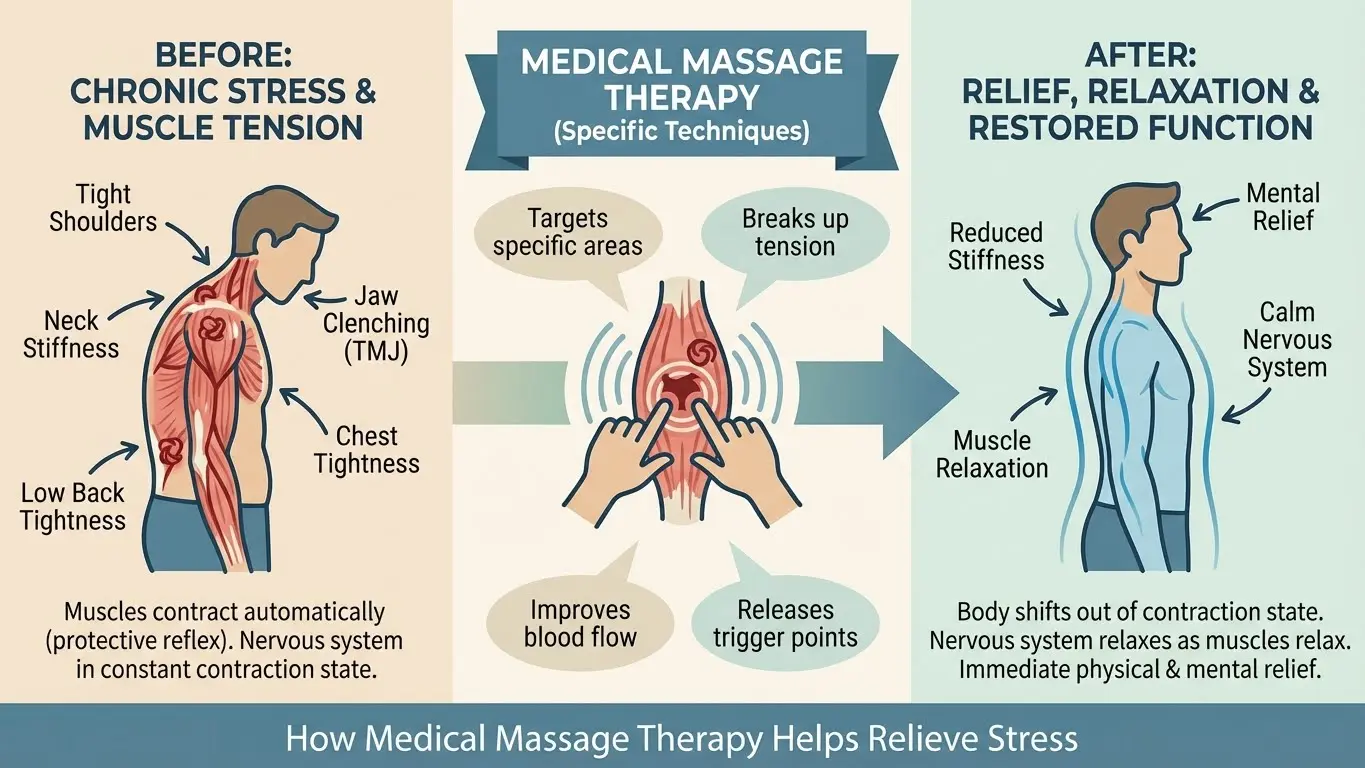
Medical massage is an outcome-focused manual therapy targeting diagnosed musculoskeletal issues, functional limitations, and chronic pain using clinical assessment and precise techniques. It reduces muscle hypertonicity, releases trigger points, improves fascial mobility, and modulates pain signaling to restore movement and reduce discomfort. Key advantages include targeted pain relief, measurable gains in range of motion and function, and integration into a rehabilitation plan with clear treatment goals. Practitioners rely on assessment findings to tailor sessions and track progress.
Medical massage often uses deeper, focused methods like neuromuscular therapy and myofascial release, driven by clinical reasoning. Being clinical, it’s frequently coordinated with other providers and may require a referral. The next section explains how it’s prescribed and how clinical plans are structured.
How Is Medical Massage Prescribed and Targeted?
Medical massage follows a clinical assessment including history, functional movement tests, and palpation to find trigger points and fascial restrictions. Clinicians set measurable goals—like lowering pain scores or improving lumbar flexion—and choose techniques aimed at identified dysfunction. If insurance coverage is possible, a physician referral or prescription can clarify frequency; otherwise, treatment proceeds as clinician-directed care. Expect documentation of findings and progress notes to guide adjustments.
This structured method focuses treatment on mechanisms causing symptoms. Targeted technique selection is central to clinical massage delivery.
Techniques Commonly Used in Medical Massage
Medical massage uses evidence-informed techniques for structural and neuromuscular problems: deep tissue work, trigger point therapy, myofascial release, and neuromuscular techniques. Deep tissue methods apply sustained pressure to remodel adhesions and lower chronic tension; trigger point therapy targets hyperirritable spots that refer pain; myofascial release restores glide across fascial planes; and neuromuscular approaches normalize tone. Each technique is applied with a documented rehabilitation goal.
Choosing the right technique depends on diagnosis, tissue response, and how it fits with other rehab elements.
Key Differences Between Medical and Traditional Massage
Medical and traditional massage differ in purpose, technique, setting, and documentation. Medical massage is clinical and goal-oriented; traditional massage is comfort-focused. Medical massage targets diagnosed conditions using modalities like trigger point release and myofascial work, including assessment, documentation, and coordination with other healthcare providers. Traditional massage emphasizes broad strokes and sensory comfort to reduce stress without formal outcome tracking. These differences affect choice and how services are billed.
Below is a concise comparison to help you decide which approach fits your needs.
| Attribute | Medical Massage | Traditional Massage |
|---|---|---|
| Primary Goal | Targeted therapeutic outcomes and improved function | Relaxation and stress relief |
| Common Techniques | Deep tissue, trigger point, myofascial release | Swedish, hot stone, aromatherapy |
| Setting | Clinical office or integrated clinic | Spa or wellness center |
| Prescription | Sometimes prescribed / documented | Generally self-scheduled |
| Insurance | May be eligible when clinically indicated | Typically self-pay |
| Outcome Measurement | Documented functional gains | Subjective relaxation and well-being |
How Goals and Approaches Differ
Medical massage aims to restore function, reduce pain signals, and support rehabilitation. Therapists use objective measures—range of motion tests, pain scales, and functional markers—to assess progress and adjust care. Traditional therapists prioritize comfort, atmosphere, and sensory experience, using subjective feedback to guide pressure. Medical sessions often include pre- and post-treatment assessments, while traditional sessions focus on uninterrupted relaxation.
These differences also influence prescription requirements and insurance considerations.
Settings, Prescriptions, and Insurance: What to Know
Medical massage is commonly offered in clinical settings where documentation and coordination with referring clinicians support medical necessity. Traditional massage usually takes place in spas or wellness centers prioritizing client comfort. Insurance rules vary—some plans require a physician referral or documented clinical notes to reimburse medical massage, while relaxation massage is generally self-pay. Coverage for medical massage is possible when it fits a documented treatment plan, but policies differ and should be verified. Clinics that help with insurance paperwork can simplify authorization.
Understanding these differences helps you plan access and costs.
How Medical Massage Helps Chronic Pain and Specific Conditions
Medical massage helps chronic pain by addressing peripheral and central contributors: it reduces muscle tension, trigger point activity, improves local circulation, and modulates nociceptive input to change how the nervous system perceives pain. For structural complaints—chronic back, neck, and joint dysfunction—medical massage complements exercise and rehabilitation to restore mobility and function. Research shows targeted manual therapy can lower pain intensity and improve functional scores as part of a multimodal plan. Expect gradual improvement across multiple visits.
Massage Therapy Efficacy for Pain & Function
This systematic review and meta-analysis evaluates massage research and its effects on pain and function. Results indicate massage therapy provides meaningful pain relief compared with sham or no treatment, supporting its use as part of multimodal care.
| Condition | How Medical Massage Helps | Expected Outcome / Example Technique |
|---|---|---|
| Chronic low back pain | Reduces paraspinal hypertonicity and improves lumbar mobility | Less pain with flexion; trigger point release |
| Chronic neck pain | Releases upper trapezius and suboccipital tension to reduce cervicogenic pain | Improved rotation and fewer headache referrals |
| Sciatica / referral pain | Decreases myofascial referral and improves pelvic–femoral mechanics | Reduced radiating pain; myofascial release |
| Fibromyalgia | Reduces local tender point sensitivity and may improve sleep | Modest pain reduction; gentle myofascial techniques |
| Post-surgical stiffness | Scar mobilization and edema management to restore range | Improved ROM; targeted soft-tissue mobilization |
Mapping conditions to techniques and realistic outcomes clarifies treatment goals and helps coordinate care with related modalities like exercise and dry needling.
At Messina Acupuncture PC, we include medical massage in personalized programs for patients with musculoskeletal and chronic pain. We provide individualized care, insurance assistance, and coordinated therapies. To discuss if medical massage is right for your condition, call 631-403-0504 to request a consultation.
Medical Massage Benefits for Chronic Back, Neck, and Joint Pain
For chronic back, neck, and joint pain, medical massage targets persistent muscle guarding, trigger points, and connective tissue restrictions that sustain pain and limit movement. Techniques like trigger point release and myofascial mobilization address referral pain patterns; deep tissue work reduces chronic hypertonicity and improves blood flow. Combined with exercise and ergonomic changes, patients commonly report lower pain scores and measurable gains in range of motion. Goals include less pain during activity, improved reach or rotation, and fewer pain flares, with regular reassessment.
Adding home exercise strengthens long-term results and helps prevent recurrence—important for post-surgical and chronic rehabilitation.
Medical Massage in Post-Surgical Recovery and Mobility
Medical massage supports post-surgical recovery by addressing scar adhesions, reducing peri-incisional stiffness, and restoring soft-tissue glide to recover joint and limb mobility. Early work focuses on gentle edema control; later stages emphasize scar mobilization and myofascial release to regain range of motion. Coordination with your surgeon and rehab team ensures timing and technique choices match healing stages; clinicians document progress and adjust intensity. Appropriately applied, medical massage can shorten rehab timelines and improve outcomes.
Ortho-Massage for Postoperative Pain & Recovery
Evidence suggests ortho-massage in the early postoperative period can reduce pain, relieve muscle tension, and support emotional wellbeing, contributing to faster functional recovery within a multidisciplinary rehabilitation plan.
Next, we’ll help you decide when medical massage is the better choice versus a relaxation-focused session.
When to Choose Medical Massage Instead of Traditional Massage
Choose medical massage when pain is persistent, progressive, or limits function. Traditional massage is better for acute stress relief, general relaxation, and occasional muscle tightness. Indications for medical massage include a diagnosed musculoskeletal issue, post-surgical rehabilitation, or persistent pain interfering with daily activities requiring a measurable treatment plan. Prefer traditional massage for wellness maintenance, stress management, or psychological relaxation. Watch for red flags—unexplained weight loss, signs of infection, or rapidly worsening neurological deficits—that require immediate medical evaluation before any manual therapy.
| Symptom / Scenario | Indicates | Recommended Choice |
|---|---|---|
| Persistent pain >3 months affecting function | Structural or chronic pain needing targeted care | Choose Medical Massage |
| Acute stress, seeking relaxation | No structural diagnosis; main goal is wellbeing | Choose Traditional Massage |
| Post-operative stiffness with surgeon clearance | Tissue-specific rehabilitation need | Choose Medical Massage |
| Occasional muscle tightness after travel | Temporary discomfort without functional loss | Choose Traditional Massage |
| Progressive neurological symptoms | Potential red flag; seek medical evaluation first | Medical evaluation before massage |
When Medical Massage Is the Better Fit
Medical massage is appropriate when you have persistent or worsening pain, measurable loss of function, recurring referral pain, or post-operative stiffness limiting activities. Signs include restricted range of motion, daily pain affecting sleep or work, or pain unresponsive to general relaxation. A clinician-led assessment identifies contributing structures and creates a targeted plan combining manual therapy, movement retraining, and coordination with other treatments. Seeking a clinical evaluation prevents overreliance on relaxation-only care when a clinical approach is required.
When Traditional Massage Is the Right Choice
Traditional massage is preferable when your primary goal is relaxation, stress relief, or occasional relief from muscle tightness with no underlying structural condition. Good candidates include people with episodic tension from short-term stress, travelers needing recovery, or anyone seeking a restorative experience to support sleep and mood. Traditional massage complements self-care and can reduce stress-related muscle guarding. If symptoms are mild, stable, and not function-limiting, a relaxation session is an efficient, low-risk choice focused on comfort and wellbeing.
Picking the right approach helps you use time and resources effectively. Next, we explain how Messina Acupuncture combines medical massage with other treatments.
How Messina Acupuncture Integrates Medical Massage with Other Therapies
At Messina Acupuncture PC, we combine medical massage with acupuncture, acupressure, and dry needling to build individualized, multimodal care plans for orthopedic and chronic pain. Integration starts with a clinical assessment: medical massage treats soft-tissue dysfunction and mobility limits, acupuncture and acupressure modulate pain pathways and support healing, and dry needling targets trigger points to normalize neuromuscular patterns. Sequencing, like using acupuncture to calm central sensitization before deeper manual work, can improve responses and accelerate rehabilitation. We emphasize personalized care, insurance assistance, and coordination across therapies to align plans with patient goals.
Patients on an integrated plan follow structured progress reviews where techniques and frequency are adjusted based on objective gains. If you’re interested in a combined approach, call Messina Acupuncture PC at 631-403-0504 to schedule a consultation with Daniel Messina and discuss insurance assistance and individualized planning.
How Acupuncture, Acupressure, and Dry Needling Work with Medical Massage
Acupuncture and dry needling primarily affect neural pain processing and local muscle tone, while medical massage restores tissue mobility and resolves adhesions. A typical session might begin with acupuncture to reduce central sensitization, proceed to targeted medical massage to mobilize restricted tissues, and include dry needling on persistent trigger points for neuromuscular reset. Acupressure is often taught as a home-care tool to maintain gains. This multimodal sequencing tends to enhance tissue response and speed functional recovery.
Care pathways use regular assessments to decide modality order and confirm functional gains as patients progress toward independent movement.
What Daniel Messina Brings to Orthopedic and Pain Care
Daniel Messina leads our clinical approach at Messina Acupuncture PC, focusing on musculoskeletal conditions and chronic pain with an orthopedic-informed, patient-centered model. We combine acupuncture, medical massage, and dry needling into tailored treatment plans addressing symptom relief and functional restoration. Our emphasis on thorough assessment and coordination with other providers supports outcomes for back, neck, joint pain, and headache disorders. Patients can expect measurable progress and practical return-to-function goals.
To schedule a targeted evaluation and discuss if medical massage is right for you, contact Messina Acupuncture PC at 631-403-0504 or schedule a consultation. We assist with insurance authorization and coordinate medical massage with acupuncture and dry needling to create individualized treatment plans for musculoskeletal and chronic pain.
Frequently Asked Questions
What should I expect during a medical massage session?
Expect a focused assessment: medical history, symptom discussion, and targeted palpation. Treatment uses techniques chosen for your needs—deep tissue work, trigger point release, or myofascial mobilization—applied for therapeutic effect. Sessions commonly run 30–90 minutes, with pressure adjusted to your feedback. Your clinician documents findings and tracks progress to guide follow-up care.
Can medical massage be covered by insurance?
Possibly. Coverage depends on your plan and medical necessity. Many insurers require a physician referral or prescription. Verify benefits with your provider; Messina Acupuncture PC often assists patients with paperwork for coverage.
How often should I receive medical massage for chronic pain?
Frequency depends on your condition and goals. Early in care, weekly sessions are common for acute symptoms. As you improve, visits may space to every two weeks or monthly. Your clinician will recommend a schedule tailored to your progress.
Are there any risks associated with medical massage?
Medical massage is generally safe, but some may experience temporary soreness or a short-term symptom increase. Certain medical conditions or recent surgeries may change what’s appropriate. Always inform your therapist about your health history, medications, and recent procedures to adapt techniques and minimize risk.
How does medical massage differ from physical therapy?
Both aim to reduce pain and restore function, but differ. Medical massage concentrates on manual treatment of soft-tissue dysfunction and pain modulation. Physical therapy typically combines manual therapy with structured exercise and movement retraining. They’re complementary—your clinician can help determine which or what combination is best for your condition.
Can I combine medical massage with other therapies?
Yes. Combining medical massage with acupuncture, dry needling, and exercise often yields better results. At Messina Acupuncture PC, we integrate these modalities into coordinated plans addressing multiple aspects of pain. Discuss your goals with your care team to build a safe, effective combined approach.